Clients participating in medication-assisted treatment typically remain in care nearly twice as long as those who do not. This evidence-based approach has been proven effective for treating both Opioid Use Disorder and Alcohol Use Disorder.
Medical Providers:
Dr. Michael Vines, MD
Alex Spritzer, FNP, CARN-AP, PMHNP
Clinical Providers:
Natalie Foster, LPC-S, MS
Last Updated: November 6, 2022
Clients participating in medication-assisted treatment typically remain in care nearly twice as long as those who do not. This evidence-based approach has been proven effective for treating both Opioid Use Disorder and Alcohol Use Disorder.
Although the behavioral therapies used in MAT may differ, only a limited number of FDA-approved medications are currently available to treat opioid addiction and alcoholism. Given the strong success rates for these conditions, researchers are now exploring medications to address other types of substance use disorders.
“Medication-Assisted Treatment (MAT) is an evidence-based approach that combines medications with counseling and behavioral therapies to deliver comprehensive, whole-person care for individuals with substance use disorders.” – SAMHSA
MAT functions differently depending on the specific medications, therapies, and type of addiction being treated.
In cases of alcohol and opioid abuse, addiction often develops when opioid receptors in the brain are activated, producing feelings of euphoria and other effects. These same receptors can also be naturally stimulated through healthy activities like exercise, which boost endorphin production.
Agonist medications activate the body’s opioid receptors, producing effects similar to those of opioids themselves.
Full agonists are substances such as oxycodone or heroin that fully activate opioid receptors, often leading to addiction. Alcohol is also considered an indirect full agonist.
Partial agonists, on the other hand, stimulate these receptors to a lesser extent, producing milder effects. These medications are commonly used in MAT to help reduce cravings and withdrawal symptoms without causing the same level of euphoria or dependence.
Antagonist medications work by blocking opioid receptors, preventing opioids from producing their usual effects.
These medications attach to opioid receptors and temporarily block the effects of agonist substances such as oxycodone or alcohol. Antagonist medications are used almost exclusively in MAT to help prevent relapse and support long-term recovery.
Pharmaceutical manufacturers have developed a range of medications that fall into either the agonist or antagonist category. Each comes in different forms and may carry its own set of potential side effects.
Let’s explore some of the most common medications used to support individuals struggling with substance use disorders and examine how each one works.
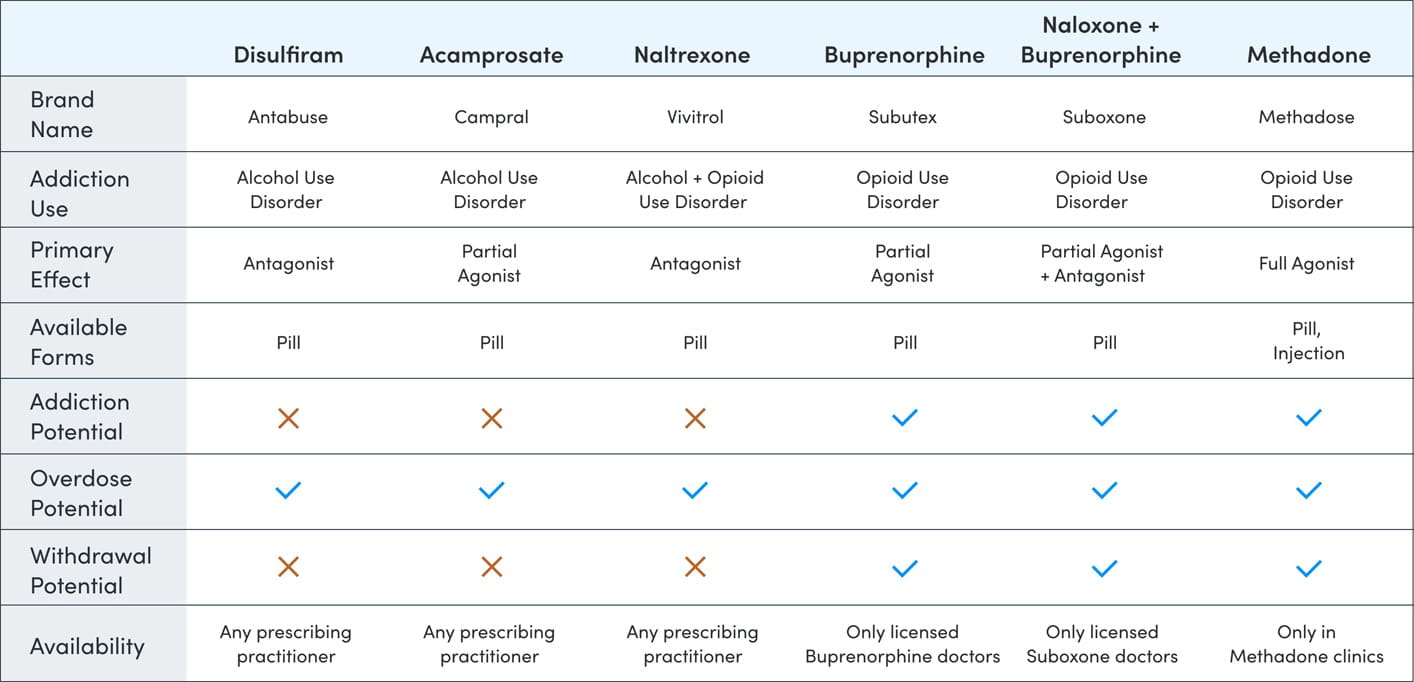
Methadone is one of the most widely used medications for treating opioid addiction. It’s also prescribed to manage severe pain in individuals with an opioid use disorder. While methadone can be an effective component of MAT, newer options are now available that carry a lower risk of dependence.
Buprenorphine is a partial opioid agonist and diminishing the effects of opioid withdrawal symptoms and cravings. Buprenorphine also has a ‘ceiling effect’ meaning once the effects of the drug have reached a certain point they will not increase as the dosage increases.
Suboxone uses both agonist and antagonist medications to simultaneously alleviate withdrawal symptoms while blocking the effects of opioids. Unfortunately, it can stay for several days in the system and can be addictive. Suddenly stopping can result in withdrawal symptoms.
Acamprosate begins working after the first dose and is primarily used to reduce cravings and urges to drink—key symptoms of alcohol withdrawal. It is approved for long-term use in individuals with Alcohol Use Disorder (AUD).
Naltrexone is one of the few medications approved to treat both opioid addiction and alcohol dependence. For individuals with Alcohol Use Disorder, it works by blocking the rewarding effects of alcohol, helping to reduce cravings and the motivation to drink.
Disulfiram changes how the body processes alcohol, leading to severe and unpleasant reactions when alcohol is consumed—even in small amounts. This form of negative conditioning can be an effective deterrent for continued drinking.
At present, there are no FDA-approved MAT medications for individuals struggling with cocaine addiction. However, given the success of MAT in treating opioid and alcohol use disorders, researchers are actively exploring potential medications to address cocaine addiction in the future.
Currently, Topiramate is approved only for the treatment of epilepsy and chronic migraines in adults. However, emerging research suggests that it may help reduce the rewarding effects of cocaine, thereby decreasing the likelihood of relapse. Because Topiramate is non-addictive, it shows promise as a potential option for treating cocaine addiction.
Baclofen, a muscle relaxant, has shown potential in helping individuals with cocaine addiction manage cravings. Research suggests it can reduce brain activity linked to cue-induced cocaine cravings, making it a promising option for supporting recovery.
Because some MAT medications can be addictive, specific support groups exist for those who develop dependence on them: Medication Assisted Recovery Anonymous.
For those in recovery, the goal is clear: lasting sobriety. Reaching that goal, however, can be challenging. By combining medication and therapy through medication-assisted treatment, clients increase their chances of achieving long-term recovery.
To truly overcome addiction, it’s essential to address any underlying conditions that may contribute to it. Dual diagnosis treatment, which integrates MAT with other therapeutic approaches, offers the most effective path for individuals facing both addiction and co-occurring mental health issues.
MAT is an evidence-based treatment approach that has been proven effective across numerous studies.
A 14-year study found that expanding access to buprenorphine and methadone resulted in a 50% reduction in heroin overdoses in Baltimore between 1995 and 2009.
Long-term studies show that MAT is effective not only in the early stages of recovery but also in maintaining lasting sobriety. After 3.5 years, 61% of clients who received MAT reported remaining drug-free.
This is a significant outcome, especially compared to behavioral interventions alone, which have an estimated 80% relapse rate.
To begin MAT, clients must first commit to their recovery and complete an evaluation process. Based on the results, a doctor will create a personalized treatment plan tailored to each client’s needs. MAT medications are typically prescribed and administered by a licensed medical professional in a clinical setting, a primary care office, or a residential rehab facility.
Provide medications that support clients in staying engaged in treatment and managing withdrawal symptoms.
Have clients participate in regular therapy to address the underlying causes of their addiction.
After a set period, gradually taper clients off the medication.
Some clients may never reach the tapering portion of medication-assisted treatment.
The cost of MAT varies depending on the medication, brand, and type of therapy involved. For example, methadone or buprenorphine treatment typically costs around $100 to $130 per week, while the brand-name version of naltrexone, Vivitrol, can exceed $1,000 per month.
Cognitive Behavioral Therapy (CBT), one of the most common therapeutic components of MAT, can cost up to $150 per session, with most therapists recommending weekly appointments.
Clients receiving treatment in inpatient or outpatient programs may face costs ranging from $3,000 to $10,000 for a 30-day program.
However, both state-funded programs and private insurance can help cover these expenses, often reducing out-of-pocket costs significantly.
A common myth about Alcoholics Anonymous suggests that participants cannot take medications while being part of the program.
While some local groups may discourage it, many AA and NA meetings accept and support individuals using MAT. These groups are not meant to provide medical advice—decisions about medication should always be made between you and your doctor.
This misconception likely comes from the outdated belief that MAT is merely replacing one substance with another.
“Neither the Alcoholics Anonymous (AA) literature nor either of its founding members spoke against using medications as a component of a recovery plan for alcohol dependence.”
–Mistie Storie, Director of Training at the Association for Addiction Professionals
Despite MAT’s proven effectiveness, not all treatment centers offer medication options for substance abuse. Although the number of facilities providing MAT is growing, availability remains limited.
In 2017, less than 40% of treatment centers offered heroin clients access to medication-assisted treatment.
One of the main reasons MAT medications aren’t more widely offered is the lingering belief that they simply replace one addiction with another.
This is a big misconception.
MAT is an evidence-based treatment approach consistently proven to help clients achieve and maintain sobriety.
Although some MAT medications have addictive potential, combining them with regular therapy allows for close monitoring and greatly reduces the risk of misuse.
Although access to MAT medications is improving, finding approved providers for certain drugs can still be challenging.
For those seeking buprenorphine, SAMHSA offers a Treatment Practitioner Locator to help you find a qualified provider nearby.
Methadone, on the other hand, must be administered at a certified outpatient clinic, and a similar locator tool is available to help you find one in your area.
If you’re looking to use MAT as one part of your journey to sobriety, Arizona IOP can help you do just that. At our Scottsdale addiction treatment centers we offer numerous MAT medications and therapy options to get you back on track.